Indice
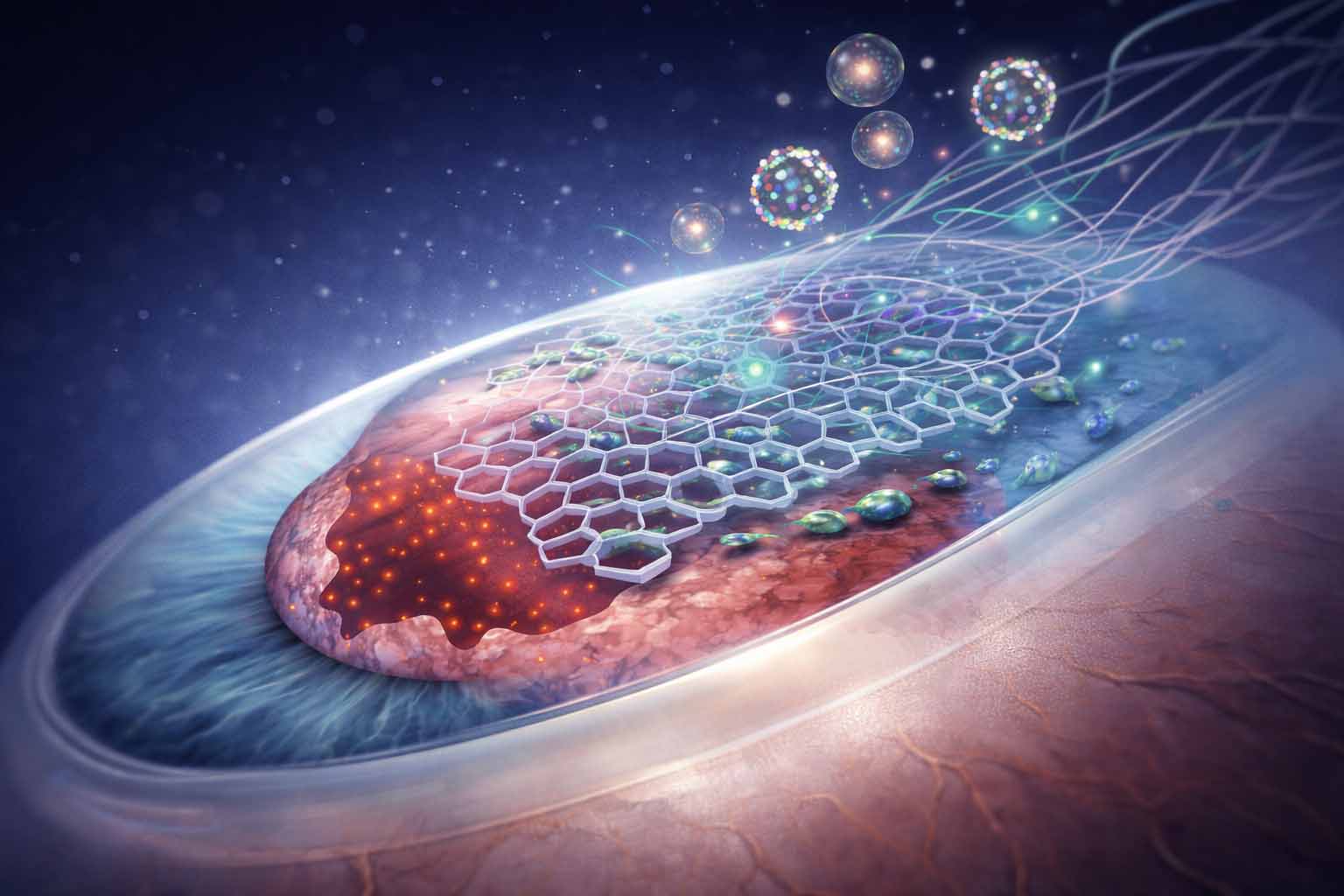
Corneal re-epithelialisation is a vital process for preserving ocular surface integrity and visual acuity. When this complex process is hindered, resulting in delayed or incomplete healing, significant clinical difficulties emerge, which can lead to persistent epithelial defects, stromal scarring, and ultimately, severe vision loss. This document examines the various clinical issues linked to slow corneal re-epithelialisation and explores innovative, forward-looking therapeutic strategies, including those utilising advanced scaffold technologies, to address these complex problems. Understanding the cellular and molecular mechanisms underlying epithelialisation is essential for developing effective interventions that promote timely and complete corneal wound closure.. Physiologically, the corneal epithelium typically heals within approximately 5 days; however, during this period, the cornea is especially vulnerable to infection, and patients often experience discomfort and a reduced quality of life. Delayed healing not only extends these risks and discomforts but can also result in more serious complications, emphasising the importance of timely and effective re-epithelialisation strategies. Persistent epithelial defects, for example, can lead to chronic inflammation, ulceration, and even corneal perforation, requiring surgical intervention to preserve the globe. Furthermore, the absence of an intact epithelial barrier exposes the underlying stromal tissue to external insults, increasing the risk of irreversible structural damage and vision loss. Current clinical approaches often face challenges with persistent defects, emphasising the urgent need for novel therapies that can not only speed up healing but also restore the cornea’s intricate architecture and function. This calls for a deeper investigation into the molecular pathways controlling corneal epithelial repair and the creation of targeted interventions that can overcome the limitations of traditional treatments. One promising direction involves developing biomimetic scaffolds that can accurately guide cellular behaviour and deliver therapeutic agents to the wound site, promoting optimal tissue regeneration. These scaffolds aim to imitate the native extracellular matrix, offering a supportive microenvironment that encourages epithelial cell migration, proliferation, and differentiation, thereby speeding up the re-establishment of a functional epithelial layer. This biomimicry is essential because wound repair involves complex interactions among various cell types, their mediators, and the extracellular matrix. Successful healing depends on restoring the epithelial cover and tissue integrity. Chronic wounds, including those of the cornea, pose a significant challenge in clinical care due to their tendency for prolonged inflammation, which hampers the transition to proliferative healing phases. This extended inflammatory response can halt the healing process, preventing the coordinated cellular actions needed for effective re-epithelialisation and tissue remodelling. The persistent inflammation often creates a vicious cycle of tissue damage and delayed healing, requiring interventions that can effectively regulate the inflammatory response and foster a pro-regenerative environment. Regenerative medicine presents promising opportunities for improving corneal wound healing through strategies such as stem cell therapy, growth factor application, and biomaterial integration to stimulate regeneration and enhance the wound microenvironment. Traditional wound management, while useful, often faces limitations in completely restoring tissue function, emphasising the need for innovative solutions beyond conventional wound dressings, which may not sufficiently offer antibacterial or antioxidant effects, or adequate mechanical support. However, recent progress in bioengineered alternative agents, including advanced wound dressing materials and innovative delivery systems, is continually enhancing the wound healing process and reducing costs, making them increasingly prominent in outpatient and perioperative management of stubborn wounds. This emphasises the vital need for advanced biomaterials and therapeutic approaches that can not only address the immediate epithelial defect but also reduce chronic inflammation and foster a regenerative rather than reparative healing response. Therefore, there is an urgent need to develop competitive therapies that go beyond conventional methods such as cell therapy, gene therapy, growth factor delivery, wound dressings, and skin grafts, which often prove unsatisfactory for all wound types. Hence, innovative smart dressings that utilise nanotechnology and advanced material science are emerging as essential tools to address these limitations, providing enhanced features for targeted drug delivery, better mechanical support, and more effective infection control. These next-generation dressings are designed to foster an optimal healing environment by incorporating sensing abilities for real-time wound monitoring and active therapeutic release. For example, nanotechnology presents a promising pathway, as nanoparticles embedded within biomaterials can impart specific beneficial properties for wound dressings, improving burn treatment and speeding up delayed healing processes. In particular, the integration of nanomaterials into wound dressings can boost their antimicrobial activity, enable sustained release of growth factors, and regulate cellular responses to promote faster epithelial migration and differentiation. Furthermore, electrospun nanofibers are especially promising for chronic wound care because of their ability to prevent microbial infiltration, sustain a balanced moisture and gas exchange environment, and stimulate cell proliferation. These nanofibers can imitate the native extracellular matrix, offering a scaffold that guides cell attachment and migration, which are vital for re-epithelialisation. Beyond their structural benefits, these advanced dressings can be engineered to include bioactive molecules or smart release systems, enabling targeted therapeutic interventions directly at the wound site. This precise delivery can enhance therapeutic outcomes and minimise systemic side effects, representing a major progress over traditional broad-spectrum treatments. This integration enables dynamic responses to changes in the wound microenvironment, such as fluctuations in pH, temperature, or inflammatory markers, through the controlled release of therapeutic agents. This capability transforms traditional passive dressings into active therapeutic platforms capable of accelerating corneal re-epithelialisation. This innovative approach can significantly shorten healing times and minimise complications, offering a more effective solution for complex corneal wounds. Among the biomaterials used to produce corneal wound healing scaffolds, silk proteins stand out owing to their exceptional biocompatibility, biodegradability, non-immunogenicity, and mechanical tunability, making them ideal candidates for creating scaffolds that promote cellular adhesion and proliferation. These properties allow silk-based scaffolds to effectively mimic the native corneal extracellular matrix, providing a superior substrate for corneal epithelial cell growth and differentiation. In particular, their ability to absorb water is crucial for maintaining a hydrated environment conducive to cellular activity and nutrient exchange, which is essential for corneal health and regeneration. In ophthalmology, silk-protein-based scaffolds are being extensively investigated for various applications, including corneal regeneration, lens, and retinal pathologies due to their ability to support cell proliferation and tissue integration. Preliminary studies have demonstrated the potential of silk fibroin scaffolds to enhance corneal re-epithelialisation by providing a supportive environment for limbal stem cell expansion and differentiation, thereby accelerating wound closure and reducing scar formation. Moreover, silk fibroin’s high permeability to oxygen and water, combined with its low thrombogenicity and inflammatory response, makes it a superior choice for corneal tissue engineering compared to other biomaterials. Preclinical and clinical data have shown promising results for corneal regeneration, often exhibiting superior outcomes in terms of transparency, structural integrity, and visual acuity compared to conventional treatments..
Riepithelializzazione corneale: sfide cliniche e terapie a base di scaffolds
La riepitelizzazione corneale è un processo fondamentale per preservare l’integrità della superficie oculare e l’acutezza visiva. Quando questo complesso meccanismo viene ostacolato, causando una guarigione ritardata o incompleta, emergono importanti difficoltà cliniche che possono portare a difetti epiteliali persistenti, cicatrici stromali e, infine, grave perdita della vista. Il presente documento esamina le varie problematiche cliniche associate alla lenta riepitelizzazione corneale ed esplora strategie terapeutiche innovative e orientate al futuro, incluse quelle che impiegano tecnologie avanzate basate su scaffold, per affrontare tali complessità. Comprendere i meccanismi cellulari e molecolari alla base della riepitelizzazione è essenziale per sviluppare interventi efficaci che promuovano una chiusura tempestiva e completa delle lesioni corneali. Fisiologicamente, l’epitelio corneale guarisce generalmente entro circa 5 giorni; tuttavia, durante questo periodo, la cornea è particolarmente vulnerabile alle infezioni, e i pazienti avvertono spesso disagio e una riduzione della qualità della vita. Una guarigione ritardata non solo prolunga questi rischi e disagi, ma può anche portare a complicanze più gravi, sottolineando l’importanza di strategie di riepitelizzazione tempestive ed efficaci. I difetti epiteliali persistenti, ad esempio, possono causare infiammazione cronica, ulcerazione e persino perforazione corneale, richiedendo un intervento chirurgico per preservare il globo oculare. Inoltre, l’assenza di una barriera epiteliale integra espone il tessuto stromale sottostante a insulti esterni, aumentando il rischio di danni strutturali irreversibili e perdita della vista. Gli approcci clinici attuali spesso incontrano difficoltà nella gestione dei difetti persistenti, evidenziando l’urgente necessità di terapie innovative che non solo accelerino la guarigione, ma ripristinino anche la complessa architettura e funzionalità corneale. Ciò richiede un’indagine approfondita delle vie molecolari che regolano la riparazione dell’epitelio corneale e la creazione di interventi mirati capaci di superare i limiti dei trattamenti tradizionali. Una direzione promettente riguarda lo sviluppo di scaffold biomimetici capaci di guidare accuratamente il comportamento cellulare e veicolare agenti terapeutici nel sito della lesione, promuovendo una rigenerazione tissutale ottimale. Questi scaffold mirano a imitare la matrice extracellulare nativa, offrendo un microambiente di supporto che stimoli la migrazione, proliferazione e differenziazione delle cellule epiteliali, accelerando così il ristabilimento di uno strato epiteliale funzionale. Questa biomimesi è essenziale poiché la riparazione delle ferite coinvolge complesse interazioni tra vari tipi cellulari, i loro mediatori e la matrice extracellulare. Una guarigione efficace dipende dal ripristino della copertura epiteliale e dell’integrità tissutale. Le ferite croniche, incluse quelle corneali, rappresentano una sfida significativa nella pratica clinica a causa della tendenza a sviluppare infiammazione prolungata, che ostacola il passaggio alle fasi proliferative della guarigione. Questa risposta infiammatoria estesa può arrestare il processo riparativo, impedendo l’azione coordinata delle cellule necessarie alla riepitelizzazione e al rimodellamento tissutale. L’infiammazione persistente genera spesso un circolo vizioso di danno tissutale e guarigione ritardata, richiedendo interventi in grado di regolare efficacemente la risposta infiammatoria e favorire un ambiente pro-rigenerativo. La medicina rigenerativa offre opportunità promettenti per migliorare la guarigione corneale attraverso strategie come la terapia con cellule staminali, l’applicazione di fattori di crescita e l’integrazione di biomateriali per stimolare la rigenerazione e ottimizzare il microambiente della ferita. La gestione tradizionale delle ferite, pur essendo utile, presenta spesso limiti nel ripristinare completamente la funzionalità tissutale, rendendo necessarie soluzioni innovative oltre i bendaggi convenzionali, che potrebbero non offrire sufficienti effetti antibatterici, antiossidanti o supporto meccanico adeguato. Tuttavia, i recenti progressi negli agenti bioingegnerizzati alternativi, inclusi materiali avanzati per medicazioni e sistemi innovativi di rilascio, stanno migliorando continuamente il processo di guarigione e riducendo i costi, rendendoli sempre più utilizzati nella gestione ambulatoriale e perioperatoria delle ferite ostinate. Questo sottolinea la necessità cruciale di biomateriali avanzati e approcci terapeutici capaci non solo di affrontare il difetto epiteliale immediato, ma anche di ridurre l’infiammazione cronica e promuovere una risposta rigenerativa piuttosto che riparativa. Vi è quindi un bisogno urgente di sviluppare terapie competitive che vadano oltre i metodi convenzionali come la terapia cellulare, genica, la somministrazione di fattori di crescita, i bendaggi e gli innesti cutanei, che spesso si rivelano insoddisfacenti per tutti i tipi di ferite. In quest’ottica, medicazioni intelligenti innovative che impiegano nanotecnologie e scienza dei materiali avanzata stanno emergendo come strumenti essenziali per superare tali limiti, offrendo caratteristiche migliorate per un rilascio farmacologico mirato, maggiore supporto meccanico e controllo più efficace delle infezioni. Queste medicazioni di nuova generazione sono progettate per creare un ambiente di guarigione ottimale, incorporando capacità di monitoraggio in tempo reale della ferita e rilascio terapeutico attivo. Ad esempio, la nanotecnologia rappresenta una via promettente: nanoparticelle incorporate in biomateriali possono conferire proprietà specifiche vantaggiose per le medicazioni, migliorando il trattamento delle ustioni e accelerando i processi di guarigione ritardata. In particolare, l’integrazione di nanomateriali nelle medicazioni può potenziare l’attività antimicrobica, consentire il rilascio prolungato di fattori di crescita e regolare le risposte cellulari per promuovere una più rapida migrazione e differenziazione epiteliale. Inoltre, le nanofibre ottenute per elettrofilatura sono particolarmente promettenti nella cura delle ferite croniche per la loro capacità di prevenire l’infiltrazione microbica, mantenere un equilibrio ottimale di umidità e scambio gassoso, e stimolare la proliferazione cellulare. Tali nanofibre possono imitare la matrice extracellulare nativa, fornendo uno scaffold che guida l’adesione e la migrazione cellulare, elementi essenziali per la riepitelizzazione. Oltre ai benefici strutturali, queste medicazioni avanzate possono essere progettate per includere molecole bioattive o sistemi intelligenti di rilascio, consentendo interventi terapeutici mirati direttamente nel sito della ferita. Questo rilascio preciso può migliorare gli esiti terapeutici e ridurre gli effetti collaterali sistemici, rappresentando un notevole progresso rispetto ai trattamenti tradizionali ad ampio spettro. Tale integrazione permette risposte dinamiche ai cambiamenti del microambiente della ferita, come variazioni di pH, temperatura o marcatori infiammatori, attraverso il rilascio controllato di agenti terapeutici. Questa capacità trasforma le medicazioni passive tradizionali in piattaforme terapeutiche attive capaci di accelerare la riepitelizzazione corneale. Questo approccio innovativo può ridurre significativamente i tempi di guarigione e minimizzare le complicanze, offrendo una soluzione più efficace per le ferite corneali complesse. Tra i biomateriali utilizzati per la produzione di scaffold per la guarigione delle ferite corneali, le proteine della seta si distinguono per la loro eccezionale biocompatibilità, biodegradabilità, non immunogenicità e adattabilità meccanica, rendendole candidate ideali per la creazione di scaffold che promuovano l’adesione e la proliferazione cellulare. Queste proprietà consentono agli scaffold a base di seta di imitare efficacemente la matrice extracellulare corneale nativa, offrendo un substrato superiore per la crescita e la differenziazione delle cellule epiteliali corneali. In particolare, la loro capacità di assorbire acqua è cruciale per mantenere un ambiente idratato favorevole all’attività cellulare e allo scambio di nutrienti, elementi essenziali per la salute e la rigenerazione corneale. In oftalmologia, gli scaffold basati su proteine della seta sono oggetto di intensa ricerca per diverse applicazioni, inclusa la rigenerazione corneale, nonché patologie del cristallino e della retina, grazie alla loro capacità di supportare la proliferazione cellulare e l’integrazione tissutale. Studi preliminari hanno dimostrato il potenziale degli scaffold in fibroina di seta nel migliorare la riepitelizzazione corneale fornendo un ambiente favorevole all’espansione e differenziazione delle cellule staminali limbari, accelerando così la chiusura delle lesioni e riducendo la formazione di cicatrici. Inoltre, l’elevata permeabilità della fibroina di seta all’ossigeno e all’acqua, unita alla bassa trombogenicità e risposta infiammatoria, la rende una scelta superiore per l’ingegneria tissutale corneale rispetto ad altri biomateriali. Dati preclinici e clinici hanno mostrato risultati promettenti per la rigenerazione corneale, spesso evidenziando esiti superiori in termini di trasparenza, integrità strutturale e acutezza visiva rispetto ai trattamenti convenzionali.
Bibliography
Abrigo, M., McArthur, S. L., & Kingshott, P. (2014). Electrospun Nanofibers as Dressings for Chronic Wound Care: Advances, Challenges, and Future Prospects [Review of Electrospun Nanofibers as Dressings for Chronic Wound Care: Advances, Challenges, and Future Prospects]. Macromolecular Bioscience, 14(6), 772. Wiley. https://doi.org/10.1002/mabi.201300561
Ambekar, R. S., & Kandasubramanian, B. (2019). Advancements in nanofibers for wound dressing: A review [Review of Advancements in nanofibers for wound dressing: A review]. European Polymer Journal, 117, 304. Elsevier BV. https://doi.org/10.1016/j.eurpolymj.2019.05.020
Andreu, V., Mendoza, G., Arruebo, M., & Irusta, S. (2015). Smart Dressings Based on Nanostructured Fibers Containing Natural Origin Antimicrobial, Anti-Inflammatory, and Regenerative Compounds [Review of Smart Dressings Based on Nanostructured Fibers Containing Natural Origin Antimicrobial, Anti-Inflammatory, and Regenerative Compounds]. Materials, 8(8), 5154. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/ma8085154
Balusamy, B., Anitha, S., & Uyar, T. (2017). Electrospun nanofibrous materials for wound healing applications. In Elsevier eBooks (p. 147). Elsevier BV. https://doi.org/10.1016/b978-0-08-101022-8.00012-0
Banerjee, K., Madhyastha, R., Nakajima, Y., Maruyama, M., & Madhyastha, H. (2021). Nanoceutical Adjuvants as Wound Healing Material: Precepts and Prospects [Review of Nanoceutical Adjuvants as Wound Healing Material: Precepts and Prospects]. International Journal of Molecular Sciences, 22(9), 4748. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/ijms22094748
Barrientez, B., Nicholas, S. E., Whelchel, A., Sharif, R., Hjortdal, J., & Karamichos, D. (2019). Corneal injury: Clinical and molecular aspects [Review of Corneal injury: Clinical and molecular aspects]. Experimental Eye Research, 186, 107709. Elsevier BV. https://doi.org/10.1016/j.exer.2019.107709
Bhattacharya, D., Ghosh, B., & Mukhopadhyay, M. (2019). Development of nanotechnology for advancement and application in wound healing: a review [Review of Development of nanotechnology for advancement and application in wound healing: a review]. IET Nanobiotechnology, 13(8), 778. Institution of Engineering and Technology. https://doi.org/10.1049/iet-nbt.2018.5312
Chen, S., Liu, B., Carlson, M. A., Gombart, A. F., Reilly, D. A., & Xie, J. (2017). Recent Advances in Electrospun Nanofibers for Wound Healing [Review of Recent Advances in Electrospun Nanofibers for Wound Healing]. Nanomedicine, 12(11), 1335. Future Medicine. https://doi.org/10.2217/nnm-2017-0017
Chouhan, D., & Mandal, B. B. (2019). Silk biomaterials in wound healing and skin regeneration therapeutics: From bench to bedside [Review of Silk biomaterials in wound healing and skin regeneration therapeutics: From bench to bedside]. Acta Biomaterialia, 103, 24. Elsevier BV. https://doi.org/10.1016/j.actbio.2019.11.050
Cullen, B., & Gefen, A. (2022). The biological and physiological impact of the performance of wound dressings [Review of The biological and physiological impact of the performance of wound dressings]. International Wound Journal, 20(4), 1292. Wiley. https://doi.org/10.1111/iwj.13960
Derakhshandeh, H., Kashaf, S. S., Aghabaglou, F., Ghanavati, I., & Tamayol, A. (2018). Smart Bandages: The Future of Wound Care [Review of Smart Bandages: The Future of Wound Care]. Trends in Biotechnology, 36(12), 1259. Elsevier BV. https://doi.org/10.1016/j.tibtech.2018.07.007
Eming, S. A., Hammerschmidt, M., Krieg, T., & Roers, A. (2009). Interrelation of immunity and tissue repair or regeneration [Review of Interrelation of immunity and tissue repair or regeneration]. Seminars in Cell and Developmental Biology, 20(5), 517. Elsevier BV. https://doi.org/10.1016/j.semcdb.2009.04.009
Feng, Y., Jupei, Z., Dong, Z., & Tang, L. (2023). Characterization, biocompatibility, and optimization of electrospun SF/PCL composite nanofiber films. REVIEWS ON ADVANCED MATERIALS SCIENCE, 62(1). https://doi.org/10.1515/rams-2022-0333
Ghafar, N. A., Jalil, N. A. A., & Kamarudin, T. A. (2021). Wound healing of the corneal epithelium: a review [Review of Wound healing of the corneal epithelium: a review]. Asian Biomedicine, 15(5), 199. Chulalongkorn University. https://doi.org/10.2478/abm-2021-0026
Gholipourmalekabadi, M., Sapru, S., Samadikuchaksaraei, A., Reis, R. L., Kaplan, D. L., & Kundu, S. C. (2019). Silk fibroin for skin injury repair: Where do things stand? [Review of Silk fibroin for skin injury repair: Where do things stand?]. Advanced Drug Delivery Reviews, 153, 28. Elsevier BV. https://doi.org/10.1016/j.addr.2019.09.003
Giorgio, G. D., Matera, B., Vurro, D., Manfredi, E., Galstyan, V., Tarabella, G., Ghezzi, B., & D’Angelo, P. (2024). Silk Fibroin Materials: Biomedical Applications and Perspectives. Bioengineering, 11(2), 167. https://doi.org/10.3390/bioengineering11020167
Gobin, A. S., Froude, V. E., & Mathur, A. B. (2005). Structural and mechanical characteristics of silk fibroin and chitosan blend scaffolds for tissue regeneration. Journal of Biomedical Materials Research Part A, 3, 465. https://doi.org/10.1002/jbm.a.30382
Graça, M. F. P., Moreira, A. F., & Correia, I. J. (2024). Application of near-infrared light responsive biomaterials for improving the wound healing process: A review [Review of Application of near-infrared light responsive biomaterials for improving the wound healing process: A review]. Journal of Drug Delivery Science and Technology, 93, 105409. Elsevier BV. https://doi.org/10.1016/j.jddst.2024.105409
Hocking, D. C. (2015). Therapeutic Applications of Extracellular Matrix. Advances in Wound Care, 4(8), 441. https://doi.org/10.1089/wound.2015.0652
Kamil, S., & Mohan, R. R. (2020). Corneal stromal wound healing: Major regulators and therapeutic targets [Review of Corneal stromal wound healing: Major regulators and therapeutic targets]. The Ocular Surface, 19, 290. Elsevier BV. https://doi.org/10.1016/j.jtos.2020.10.006
Kolimi, P., Narala, S., Nyavanandi, D., Youssef, A. A. A., & Dudhipala, N. (2022). Innovative Treatment Strategies to Accelerate Wound Healing: Trajectory and Recent Advancements [Review of Innovative Treatment Strategies to Accelerate Wound Healing: Trajectory and Recent Advancements]. Cells, 11(15), 2439. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/cells11152439
Li, P., Chen, S.-C., Hsueh, Y., Shen, Y.-C., Tsai, M., Hsu, L., Yeh, C., Chen, H., & Huang, C. (2020). Gelatin scaffold with multifunctional curcumin-loaded lipid-PLGA hybrid microparticles for regenerating corneal endothelium. Materials Science and Engineering C, 120, 111753. https://doi.org/10.1016/j.msec.2020.111753
Lyu, Y., Liu, Y., He, H., & Wang, H. (2023). Application of Silk-Fibroin-Based Hydrogels in Tissue Engineering [Review of Application of Silk-Fibroin-Based Hydrogels in Tissue Engineering]. Gels, 9(5), 431. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/gels9050431
Mazurek, Ł., Szudzik, M., Rybka, M., & Konop, M. (2022). Silk Fibroin Biomaterials and Their Beneficial Role in Skin Wound Healing [Review of Silk Fibroin Biomaterials and Their Beneficial Role in Skin Wound Healing]. Biomolecules, 12(12), 1852. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/biom12121852
Mbese, Z., Alven, S., & Aderibigbe, B. A. (2021). Collagen-Based Nanofibers for Skin Regeneration and Wound Dressing Applications [Review of Collagen-Based Nanofibers for Skin Regeneration and Wound Dressing Applications]. Polymers, 13(24), 4368. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/polym13244368
Miguel, S. P., Figueira, D. R., Simões, D., Ribeiro, M. P., Coutinho, P., Ferreira, P., & Correia, I. J. (2018). Electrospun polymeric nanofibres as wound dressings: A review [Review of Electrospun polymeric nanofibres as wound dressings: A review]. Colloids and Surfaces B Biointerfaces, 169, 60. Elsevier BV. https://doi.org/10.1016/j.colsurfb.2018.05.011
Moradifar, F., Sepahdoost, N., Tavakoli, P., & Mirzapoor, A. (2024). Multi-functional Dressings for Recovery and Screenable Treatment of Wounds: A review [Review of Multi-functional Dressings for Recovery and Screenable Treatment of Wounds: A review]. Heliyon, 11(1). Elsevier BV. https://doi.org/10.1016/j.heliyon.2024.e41465
Pastar, I., Stojadinović, O., Yin, N., Ramirez, H., Nusbaum, A. G., Sawaya, A. P., Patel, S., Khalid, L., Isseroff, R. R., & Tomic‐Canic, M. (2014). Epithelialization in Wound Healing: A Comprehensive Review [Review of Epithelialization in Wound Healing: A Comprehensive Review]. Advances in Wound Care, 3(7), 445. Mary Ann Liebert, Inc. https://doi.org/10.1089/wound.2013.0473
Pormohammad, A., Monych, N. K., Ghosh, S., Turner, D., & Turner, R. J. (2021). Nanomaterials in Wound Healing and Infection Control [Review of Nanomaterials in Wound Healing and Infection Control]. Antibiotics, 10(5), 473. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/antibiotics10050473
Rashid, A. (2024). Untitled. https://doi.org/10.55277/researchhub.vq5dnd6h
Shimizu, Y., Ntege, E. H., & Sunami, H. (2022). Current regenerative medicine-based approaches for skin regeneration: A review of literature and a report on clinical applications in Japan [Review of Current regenerative medicine-based approaches for skin regeneration: A review of literature and a report on clinical applications in Japan]. Regenerative Therapy, 21, 73. Elsevier BV. https://doi.org/10.1016/j.reth.2022.05.008
Stoica, A. E., Chircov, C., & Grumezescu, A. M. (2020). Nanomaterials for Wound Dressings: An Up-to-Date Overview [Review of Nanomaterials for Wound Dressings: An Up-to-Date Overview]. Molecules, 25(11), 2699. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/molecules25112699
Theoret, C. L. (2004). Update on wound repair. Clinical Techniques in Equine Practice, 3(2), 110. https://doi.org/10.1053/j.ctep.2004.08.009
Wiegand, C., Hipler, U., Elsner, P., & Tittelbach, J. (2021). Keratinocyte and Fibroblast Wound Healing In Vitro Is Repressed by Non-Optimal Conditions but the Reparative Potential Can Be Improved by Water-Filtered Infrared A. Biomedicines, 9(12), 1802. https://doi.org/10.3390/biomedicines9121802